by Henry Lambert
The dreaded Lisfranc injury. There has been a lot of interest and discussion surrounding this
injury after Chet Holmgren, the number two 2022 NBA draft pick suffered a ‘Lisfranc’ ruling
him out for his entire rookie season.
Early and accurate diagnosis is essential to ensure successful outcomes and minimise
ongoing disability. Regaining adequate strength and stability through the midfoot is critical
to a swift and successful return to sport.
A thorough, objective based rehabilitation program guided by a professional with
experience managing this injury will maximise the likelihood of returning to full athletic
performance.
What is a Lis Franc injury?
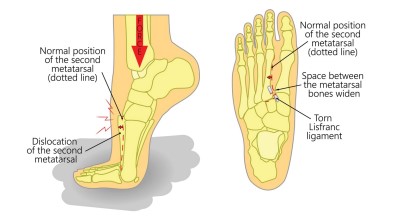
A Lisfranc injury is a disruption to the ligaments which support articulation between the
medial cuneiform and the 2nd metatarsal bones of the midfoot. This articulation is made up
of three ligaments, the dorsal ligament, the plantar ligament and the interosseous ligament.
However, any interruption to the intercuneifrom joints or any of the tarsometatarsal joints
may also be classed as a Lisfranc injury. Severity can range from partial sprains with no
displacement to complete tears with separation of the first and second metatarsals.
Stability in this area of the foot is critical, so any interruption will be catastrophic in the
athletic population.
How do they occur?
On the sporting field, these injuries usually occur with a hyper plantarflexion (toes down)
and rotational force. Often the athlete reports being tackled while their heel is up in
plantarflexion. Outside of sport, these injuries usually occur when the toes become trapped
involving the wheel of a car or forklift.
Diagnosis
Diagnosis is usually made with high clinical suspicion and appropriate imaging. The acutely
injured patient will often;
- Describe an injury mechanism as above
- Be unable to weight bear, particularly during the push off phase of walking
- Have swollen midfoot + plantar ecchymosis (bruising under the midfoot region)
- Have a positive piano key test and pain with combined eversion abduction while the calcaneus is held still
- Be painful to palpate over the midfoot region
In the sub-acute to chronic presentation, the athlete will describe a lack of power/instability
during push off and pain through the midfoot region that has not improved following an
acute incident.
Plain X-ray is enough to confirm the diagnosis. Features too observe in an isolated Lisfranc
injury include;
- Separation between 1st and 2nd metatarsals > 2mm
- Separation between the cuneiforms
- Separation between the medial cuneiform and 2nd metatarsal
- A disruption in the line between the medial boarder of the second metatarsal and the intermediate cuneiform
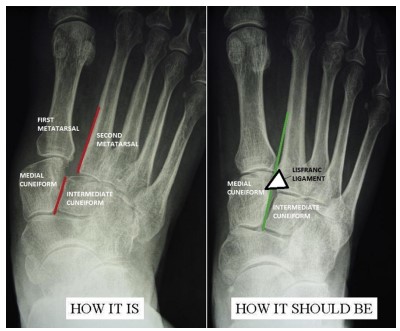
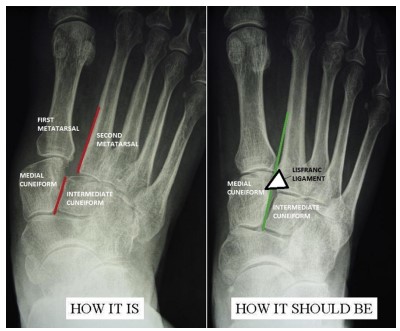
Weight bearing CT scan in full dorsiflexion may be useful for the injuries that are less
obvious on x-ray. Cross sectional area between 2nd metatarsal and medial cuneiform should
be no greater than 9% compared to the other side.
Early Management
In many cases, this injury is managed surgically with open reduction internal fixation. This
hardware is often removed at 6-12 weeks post op. Progressive surgeons are starting to use a
‘tight-rope’ like surgery, similar to the technique used in syndesmosis repair to act like a
synthetic ligament. Patients will then be placed in a blackslab or CAM walker for 6 weeks
non weight bearing.
Stable injuries should be treated non surgically, usually with 6 weeks non weight bearing in
a CAM walker. Once the boot has been removed, rehabilitation is similar to the surgical
approach.
Mid to Late Stage Management
Physiotherapy will be heavily involved during this stage of rehab. Management consists of
strengthening the intrinsic foot muscles whilst gently promoting normal range of motion
through the foot and ankle. Range of motion through all ankle and foot joints are often
impaired due to the immobilisation phase.
Intrinsic and extrinsic foot muscles are strengthened in a heel down position before gently
progressing into a plantarflexed position (up on toes, heel up) where the Lisfranc complex is
under higher loads. Guidance by a physiotherapist experienced in managing these injuries is
critical.
During this stage, it is also important to regain strength lost during immobilisation around
the knees and hips to facilitate optimal return of proper biomechanics. Isometric
dynamometry (such as the KangaTech 360 platform) should be used to identify weaknesses
and measure progress. Additionally, cardiovascular fitness should be maintained using
appropriate cross training.
Late stage rehab involves more dynamic exercises which are sport specific such a hopping,
jumping, landing, sand running and high-level stability tasks.
Running is reintroduced once the patient has achieved adequate strength, stability and
biomechanics through their midfoot, has adequate range of motion (particular focus on
dorsiflexion) and is pain free on walking, calf raises and hopping.
Prognosis and Return to Play
Return to play can vary significantly depending on the grade of injury and the approach to
management. Athletes with a low-grade injury (minimal displacement) managed with a
‘tight-rope’ repair can return to play within 2-4 months. An Australian study (Sullivan et al.
2022) found return to competition times with tightrope repair in 12 elite athletes was
between 12-16 weeks. Low grade injuries managed conservatively (moon boot) may take
between 4-10 months to return to play.
Complex Lisfranc injuries will often take the best part of 12 months to return to play. Open
reduction internal fixation surgical management is used with these complex cases. In some
instances, these athletes never return to their previous level of performance.
McHale et al reviewed Lisfranc injuries in the NFL from 2000-2010 and found the average
return to play time was 11 months, however almost 10% retired after sustaining this injury.
A thorough, objective based rehabilitation program guided by a professional with
experience managing this injury will maximise the likelihood of returning to full
performance.